Activity
Mon
Wed
Fri
Sun
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
What is this?
Less
More
Memberships
Castore: Built to Adapt
768 members • Free
Landmine University
17 members • Free
Endless Evolution w/ Duffin
2.5k members • Free
8 contributions to Castore: Built to Adapt
Most Fatigue Advice Fails Because It Confuses These Two Very Different Problems
Low energy is one of the most common complaints in medicine, coaching, and everyday life, yet it is one of the least precisely understood. People describe it as fatigue, burnout, brain fog, weakness, lack of motivation, or feeling “offline.” Athletes feel it when they cannot train. Patients feel it when they cannot work. High performers feel it when discipline no longer works. The problem is that “low energy” is not a diagnosis. It is a surface description of a system-level failure, and two people can experience nearly identical symptoms while the underlying biology is completely different. Treating them the same way helps one person and harms the other. To understand low energy correctly, you have to stop asking how to boost energy and start asking why energy is being limited in the first place. At the deepest level, there are two dominant failure modes. In one, the body cannot produce enough energy. In the other, the body is deliberately suppressing energy production. The first is mitochondrial damage, a capacity problem. The second is inflammatory inhibition, a regulatory decision. One is a broken engine. The other is a functioning engine with the brakes applied. Subjectively they feel similar. Biologically they are opposites. Everything that follows depends on recognizing which one you are dealing with. A simple model helps. Imagine the body as a car. The mitochondria are the engine. They take fuel and oxygen and convert them into usable energy in the form of ATP. Inflammation acts like the central control computer, deciding how much power the engine is allowed to produce. If the engine is damaged, pressing the accelerator does little. If the computer is limiting output, the engine could perform, but is being intentionally restrained. In both cases the car goes slow. Only one responds to pushing harder. Mitochondria exist inside nearly every cell and are responsible for producing ATP, the molecule that powers muscle contraction, nerve signaling, hormone synthesis, immune regulation, tissue repair, and cognition. Without adequate ATP, nothing in the body functions well. Energy production depends on intact mitochondrial membranes, functioning enzymes, proper redox balance, sufficient oxygen delivery, and a steady supply of micronutrients. When any part of this system is damaged, the maximum amount of energy the body can generate drops. This is not a motivational issue. It is a hard ceiling.
Your Muscles and Brain Aren’t Breaking — Their Membranes Are
Most people think of seafood as “protein plus omega-3s.” That framing is incomplete. What actually makes marine foods unique is not just the fats they contain, but how those fats are organized inside membranes. This organization happens through phospholipids, and phospholipids determine how cells breathe, signal, contract, recover, and adapt. If you want to understand muscle performance, brain health, recovery, inflammation, or aging, you have to understand membrane biology first. This article will walk through what phospholipids are, why membranes matter more than isolated nutrients, and how mussels, mackerel, sardines, and anchovies differ at a molecular level. We’ll move from beginner-friendly analogies to mitochondrial signaling and redox chemistry, and end with clear takeaways for clinicians and strength coaches. Start with a simple picture. Every cell in your body is wrapped in a membrane. Every mitochondrion inside that cell is also wrapped in membranes. These membranes are not passive walls. They are active, dynamic surfaces where energy transfer, signaling, and adaptation happen. The material those membranes are made of determines whether signals flow cleanly or break down into noise. Phospholipids are the structural units of membranes. Each phospholipid has a “head” that interacts with water and “tails” that interact with fat. When billions of them line up, they form a flexible, semi-fluid surface that proteins, receptors, enzymes, and ion channels embed into. If the phospholipid composition is poor, those proteins still exist, but they don’t work properly.A useful analogy is a racetrack. The engines (mitochondria) and drivers (enzymes) matter, but if the track surface is cracked or unstable, performance suffers no matter how strong the engine is. Phospholipids are the track surface. There are several major classes of phospholipids relevant to human physiology. Phosphatidylcholine (PC) provides membrane structure and transport. Phosphatidylethanolamine (PE) contributes to curvature and mitochondrial dynamics. Phosphatidylserine (PS) is critical for signaling, especially in neurons and muscle activation. Then there are plasmalogens, a special subclass with a unique chemical bond that gives them antioxidant and redox-buffering properties.
Why Your Tendons Aren’t Weak — Your Blood Vessels and Recovery Signals Are
This article is about something most people sense intuitively but rarely understand mechanistically: why the right kind of mechanical load, paired with the right biochemical environment, can rebuild tissue, protect blood vessels, and make the whole system more resilient instead of more inflamed. We are going to walk from the “what” all the way down to the molecular “how,” and then back up to what this actually means on the gym floor and in a clinic. At the center of this story are three players that usually live in separate conversations: tendon loading, endothelial health, and pro-resolving lipids. When you connect them, you get a very different way of thinking about injury prevention, recovery, and long-term performance. Let’s start with the big picture. Your body is not a collection of parts. It is a sensing network. Every cell is constantly asking two questions: “What forces am I under?” and “What chemical signals are present?” Adaptation only happens when those two answers line up. Mechanical load without biochemical support creates damage and inflammation. Biochemical support without mechanical signal creates fragility. The magic happens when mechanical information and biochemical resolution arrive together. This is why some people get stronger tendons and healthier arteries from training, while others just accumulate pain, stiffness, and vascular wear. Now let’s zoom in. Tendons exist to transmit force. They are not passive ropes. They are living tissues made mostly of collagen fibers, water, and specialized cells called tenocytes. Tenocytes are professional listeners. They listen to tension. When you load a tendon, especially with slow isometrics or controlled eccentrics, you deform the collagen matrix. That deformation is not damage by default. It is information. At the cell membrane level, tenocytes sense this deformation through structures called integrins. Integrins are like molecular hands that connect the outside scaffold of the cell to the inside skeleton made of actin. When tension increases, integrins change shape and activate focal adhesion kinase, often shortened to FAK. FAK is a signaling hub. Once it turns on, it tells the nucleus, “We are under load. Reinforce the structure.” Downstream of FAK, pathways like MAPK and ERK activate genes involved in collagen synthesis, matrix remodeling, and cytoskeletal organization. This is how tendons get thicker, stiffer, and more resilient.
You’re Fit, Lean… and Foggy? The Hidden Form of Insulin Resistance No One Is Talking About.
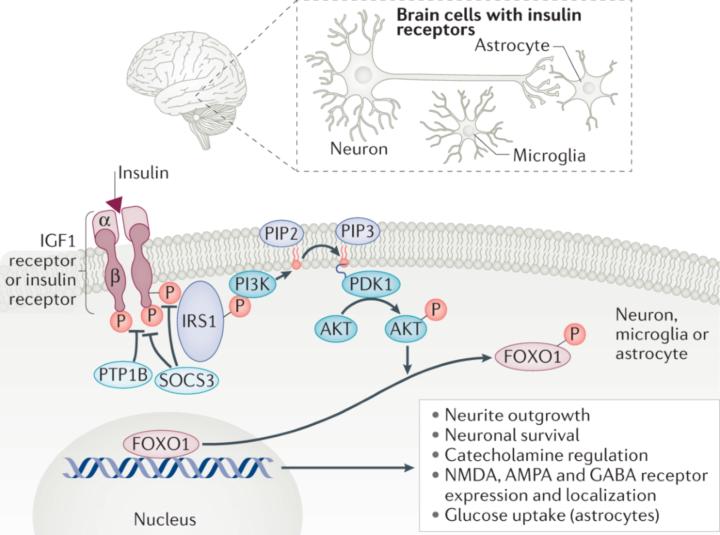
Thanksgiving has a way of slowing life down just enough for you to actually notice what’s been happening underneath all the noise. You sit with people you love, share a big meal, breathe for the first time in weeks, and suddenly you’re able to feel things you usually ignore. Maybe this year, in that moment of stillness, you noticed something strange: your body feels strong, your training is dialed in, your glucose looks perfect… but your brain doesn’t match how good the rest of you feels. Maybe you felt foggy after a meal, mentally slower than usual, overwhelmed for no reason, or just “not as sharp,” even though everything on paper says you’re metabolically healthy. If that sounds familiar, you are not alone and there’s a real physiological explanation behind it. How can someone be physically insulin-sensitive yet mentally sluggish? How can your muscles get the fuel they need while your brain feels like it’s running on fumes? This article is written for you, to answer exactly that question. Central insulin resistance is the phenomenon where your brain becomes insulin-resistant even when the rest of your body remains highly insulin-sensitive. Many people experience this as a strange mismatch: they feel physically strong, metabolically healthy, and steady during training, yet their cognition feels foggy, slow, unpredictable, overwhelmed, or “under-powered.” This article explains why that happens, what the mechanisms are, how to recognize the patterns, and how to fix them, using simple language without sacrificing the biochemical accuracy that clinicians and experts expect. The first thing to understand is that the brain handles insulin differently from the rest of the body. Your muscles and liver respond directly to insulin in the bloodstream. The brain does not. For insulin to have any effect in the brain, it must cross the blood–brain barrier, bind to receptors on neurons, activate the PI3K-Akt pathway, and allow neurons to take up and use glucose. If anything disrupts that sequence, neurons will be under-fueled even if the entire rest of the body is functioning perfectly. This is why someone can have excellent fasting glucose, low insulin, perfect CGM curves, and still feel terrible cognitively. The brain can become insulin-resistant before the body gives any signal.
Why Coffee and Fatty Foods Can Send You Running: A Deep Dive Into Gut–Mitochondrial Signaling
Most people have experienced it at some point: you sip your morning coffee or eat a rich, fatty meal, and within minutes you feel the urgent need to find a bathroom. What feels like a quirky reflex is actually a highly coordinated biochemical cascade that ties together gut chemosensors, mitochondrial redox signaling, and the autonomic nervous system. Understanding it not only explains the “coffee poops,” but also reveals a deeper logic about how the body manages energy, digestion, and balance. Coffee contains caffeine and chlorogenic acids, both of which stimulate gastrin and cholecystokinin (CCK). These hormones tell the stomach to empty faster and nudge the colon to get moving. Fatty foods add another layer: long-chain fatty acids in the small intestine trigger a surge of CCK, leading to gallbladder contraction (bile release) and pancreatic enzyme secretion. CCK also excites vagal afferents the gut’s way of phoning the brainstem to say, “Make room, something’s coming through.” The bile salts released to digest fats don’t just emulsify lipids. They also activate FXR and TGR5 receptors. TGR5 in particular lights up enteric neurons, ramping up motility. Pancreatic lipase breaks fats into free fatty acids and monoacylglycerols, which in turn hit GPR40/120 receptors, further fueling CCK and GLP-1 release. Meanwhile, caffeine blocks adenosine A1 receptors, removing a natural brake on motility and keeping cAMP signaling elevated. In essence, coffee and fats act like two friends teaming up one pushes down on the gas pedal, the other disables the brakes. Normally, digestion is a dance between the parasympathetic (rest-and-digest) and sympathetic (fight-or-flight) branches of the autonomic nervous system. Coffee and fats tilt that balance. Parasympathetic vagal activity spikes, releasing acetylcholine into the enteric nervous system, which activates M3 muscarinic receptors on gut smooth muscle. The result is strong peristalsis. Sympathetic tone temporarily relaxes, lowering sphincter control and letting the colon empty faster. The gastrocolic reflex, which is usually a subtle background process, gets supercharged. That’s why the urge can feel instantaneous.
1-8 of 8
@matt-spaid-2708
Founder/Head Coach at Operation Antifragile
Power Athlete Certified Coach and Adaptive Athlete Level 1 Trainer.
Mental Health Advocate
Strongman dude
Active 20h ago
Joined Aug 4, 2025
Powered by