Activity
Mon
Wed
Fri
Sun
Nov
Dec
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
What is this?
Less
More
Memberships
Sawinery Woodworking Guild
1.5k members • Free
Agten Radiology Patreon
73 members • Free
MSK Radiology
2k members • Free
Pre-RadPodSquad
51 members • Free
RS
Radiology School
52 members • $5/m
30 contributions to MSK Radiology
Knee pain
Women 65 y.o. Referred due to pain in the femoropatellar region. Cartilage thinning in the patella, probably some chondrocalcinosis (I don't have X-Ray) due to the diffuse low signal of the cartilage. I was wondering what you think about the low signal stuf in the suprapatellar recess. Sinovitis? Maybe fat similar to lipoma arborescens? Blood deposits? Thank you guys in advance https://www.cmrad.com/cases/1416384805
0 likes • Jul 29
I think that low signal stuff int he suprapatellar recess could be prominent synovium. I'm sometimes careful to use the synovitis, because it implies an inflammation and totally depends on who ordered the study. Some primary care doc or PA may get super worried and call you and ask about what they should do next etc. Technically you'd need contrast to get a better idea of synovitis etc. They also could be prominent synovial folds, but I feel like synovial folds are typically just a single fold that is thick and long, and this stuff is less organized and more in thin strands. I think this person has a decent amount of partial thickness cartilage loss mainly at the patella. That could be from various things; just by looking, it doesn't seem like they have obvious patellar maltracking morphology.
Tear of SSP and ISP?
Female 50 y.o. There is known tear of supraspinatus and infraspinatus tendon. Patient has frozen shoulder. Q1: It looks like incomplete full thickness tear of SSP, with rupture of the posterior aspect of tendon and extending to the infraspinatus? I am guessing there is tendinosis of the anterior aspect of SSP tendon but without rupture? Q2: Why the bone marrow of humerus is so bright on T2 SPAIR with prominent vessels? https://www.cmrad.com/cases/1786240110
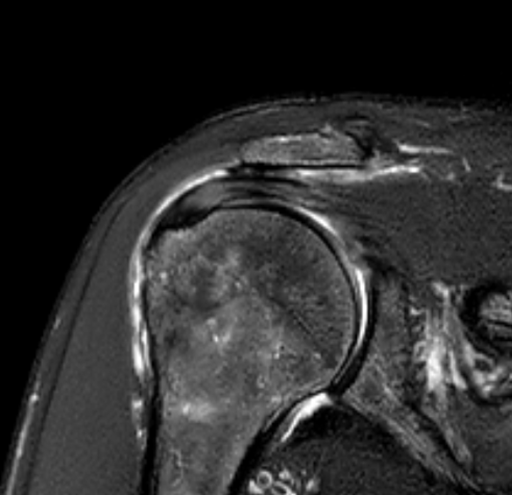
1 like • Jul 29
I think this is a full-thickness tear mainly involving the anterior infraspinatus tendon but also some of the posterior suprapsinatus junctional fibers. I don't see how you could find any intact bursal or articular surface fibers. Definitely some underlying tendinosis. What further suggests this is more so infraspinatus is that there is already some degree of muscle bulk loss and infiltration into the infraspinatus, not much elsewhere. I agree the humeral head cysts are related to traction enthesopathy, particularly related to the infraspinatus, also noting there is some intrasubstance fluid/cyst formation dissecting into the infraspinatus muscle.
Radiology's Most Toxic Belief
How many MSK cases do you report per day? I know a teleradiologist who reports 150. Yes, 150 MSK MRIs in a single day. Is this reckless? Or is it a skill we can learn? When I first asked this question on LinkedIn, it was quite controversial. People told me that it was a "slippery slope" and that "speed kills". I disagree. There are academic studies that found NO CORRELATION between speed and accuracy. In fact, I think this attitude that it is dangerous to even TALK about speed is the most toxic belief in radiology. I explain why in the article https://www.skool.com/mskrad/classroom/bed46d1f?md=7a1001df58d143aa89777d2118cc0756 How do you think about speed in radiology? I'd love to hear what you think. It's a subject that I'm passionate about and I'm always curious to hear more perspectives. Thanks! Chris
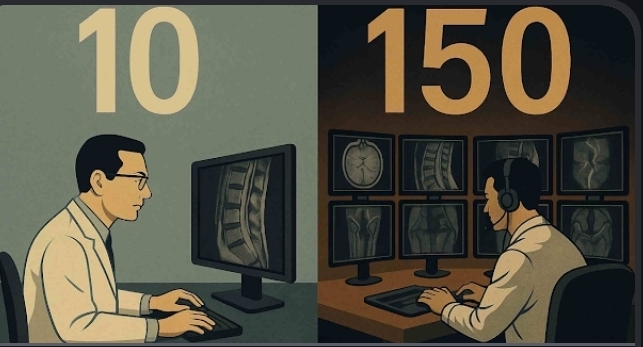
0 likes • Jul 28
I really appreciate the conversation around speed, as it almost seems taboo to discuss openly, but we all feel the pressure to read faster everyday. In fact, the pressure to read faster may be the single most pervasive feeling for radiologists. Events like the radiology olympics are a fun way to explore this topic in a safe environment. Dr. Agten's discussion and approach to the topic of speed is a welcome (and necessary) dialogue. Thank you @Christoph Agten. However, 150 MR cases a day is absolutely absurd in any setting. I can read about 50-60 cross-sectional plus 40-50 radiographs on a fast day, which includes some straightforward easy/normal knee and shoulder cases as well as some pre-operative CT cases, which are a breeze. We do have a decent amount of complex joints, such as hands and thumbs, and lots of postoperative cases and a few tumors here and there. All of that makes for an interesting and variable case load, but obviously does slow us down. I also get many phone calls throughtout the day, including questions about protocols and prior cases (even some from patients :)). Our fastest reader can probably read upwards of 60-70 xsectional cases per day, but he misses a decent amount. So, to reiterate, 150 MR is absurd and completely dangerous and in fact, I don't believe it. I'm still early in my career, but I've reached a point where I'm more interested in increasing speed via things like improving hanging protocols, faster access to priors, and better ergonomics, etc. In that regard, I'd like to start a discussion about what technology people use to improve their speed. What desk and microphone setup do you use and what are some tools you use to help your speed and comfort while reading?
Hip labral tears Lecture now on youtube
I published my Vancouver bone squad lecture on Youtube, in case you missed it https://youtu.be/aI2GbyV2KAg
1-10 of 30
Active 17d ago
Joined Sep 15, 2022
Powered by





