Activity
Mon
Wed
Fri
Sun
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
What is this?
Less
More
Owned by Harsh
The #1 Community to Land Spring Weeks, Internships & Grad Roles — Guaranteed.
Memberships
Doctri Academy
2 members • Free
Doctri
258 members • $49/month
Finance Fast Track Academy
3.8k members • $5/month
7 contributions to Doctri
🧠 UCAT Tip of the Day: Master the Art of Skipping
One of the biggest mistakes students make in the UCAT is getting stuck on hard questions. Remember: the UCAT is a speed test, not a perfection test. ✅ If a question is taking more than 30 seconds and you’re not making progress — flag it and move on. ✅ You can always come back if you have time at the end (and you often will if you don’t waste time early). ✅ Skipping is a strategy, not a failure. Top scorers don’t answer every question perfectly — they manage their time ruthlessly and play the percentages. 🚀 Train yourself to spot time traps and build speed, not just accuracy. 💬 What’s your biggest time-waster in the UCAT right now? Drop it below — let’s solve it together. ❓Stay tuned for tomorrow’s UCAT practice questions – straight from our mentors.
Mark Scheme for MMI Question of the day is out! 📖
The mark scheme for the ethical question can now be found on the interview questions discussion thread. Mark your answers and see what you got! Post your thoughts and any questions on the thread You got this👊
MMI Question of the Day🩺
MMI question of the day is out! Today's question is covering data interpretation 📊. This is a really easy station if you have done enough practice! 😆 Head over to the interview questions thread and write your answers in the comment section and discuss how you would go about answering this in an interview ✍️. Answers will be posted tomorrow so keep an eye out! 👀 You got this👊
3
0
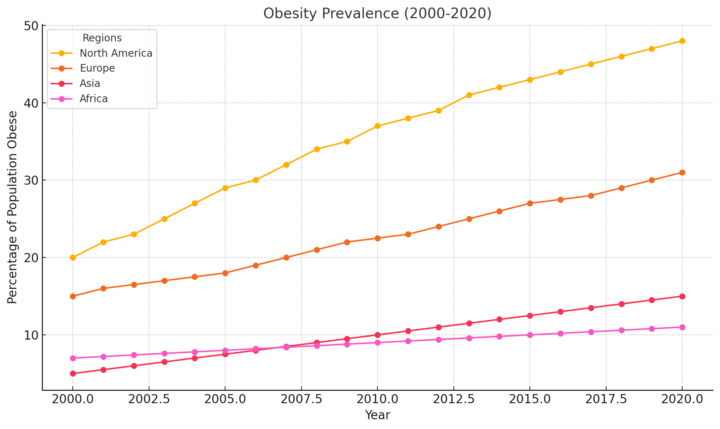
MMI Question of the day: Data interpretation📊
1) What trends do you observe in the obesity prevalence for the different regions shown on the graph between 2000 and 2020? 2)Which region shows the most significant increase in obesity prevalence, and what might be the reasons behind this trend? 3)Compare the trends for North America and Europe. Why might the increase in obesity prevalence differ between these two regions? 4)What strategies could governments in regions like North America and Europe implement to address the obesity epidemic
3
0
Mark Scheme for Epilepsy Question
1. Introduction and Initial Approach - Demonstrate professionalism and empathy: Use open body language and a calm, non-judgmental tone. Acknowledge the patient’s concerns: “I understand that this situation must be very stressful for you, and I’m here to support you.” - Build rapport and establish trust: Ensure the patient feels heard by actively listening to their concerns. Use reflective listening: “I can see how the thought of losing your job and the financial impact is deeply worrying.” 2. Assess the Situation - Clarify details about the seizures: Ask about the frequency, severity, and timing of recent seizures. Inquire about potential triggers, compliance with medication, and any recent changes in health or stress levels. - Understand the patient’s driving patterns: Explore when and where they are driving: “Can you help me understand how often you drive and for what purposes?” - Assess the patient’s insight: Gauge their understanding of the risks of driving after seizures. 3. Explain Legal and Ethical Obligations - Educate the patient about legal responsibilities: Clearly outline their obligation to inform the DVLA about their seizures: “By law, if someone has had a seizure, they must inform the DVLA because it can impact their ability to drive safely.” - Highlight the risks of non-compliance: Discuss potential consequences if they do not inform the DVLA, such as legal penalties, invalidation of insurance, or causing harm to themselves or others. - Explain the GP's duty of care: Emphasize the ethical obligation to protect public safety: “As your GP, it’s my responsibility to ensure both your safety and the safety of others on the road.” 4. Address Patient Concerns - Acknowledge financial and emotional worries: Validate their concerns about losing their job and financial instability. Offer a compassionate response: “I understand that losing your license can feel like losing your independence and livelihood, but let’s explore how we can support you through this.”
5
0
1-7 of 7


