Activity
Mon
Wed
Fri
Sun
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan
Feb
What is this?
Less
More
Memberships
MRCS OSCE (Part B)
176 members • $10/month
35 contributions to MRCS OSCE (Part B)
Congratulations to those who passed
We are thrilled to congratulate @Fathalrahman Gadallah @Mohammed Sadig for passing their Exam. Good luck with the rest of your journey.✅
Feedback 🚀
Meeting with one of our students who passed the MRCS PART B EXAM👌🩺🚀 Congratulation👏🏻👏🏻 Join us now to start your journey 🚀


Immunohistochemistery test IHC
Immunohistochemistry (IHC) is a laboratory technique that uses antibodies to detect specific proteins (antigens) within cells in a tissue sample. by identifying specific molecules (markers) that distinguish between different types and subtypes of the disease. What it does: - IHC uses antibodies designed to bind to specific proteins (antigens) within a tissue sample. - The antibody-antigen reaction is visualized using various methods, such as enzymes or fluorescent dyes, which allow pathologists to see where the target protein is located within the tissue. - IHC is particularly useful in diagnosing cancers by identifying specific proteins that indicate the type and origin of the cancer. How IHC performed : 1. Tissue preparation:Tissue samples are prepared and fixed (often with formalin) to preserve their structure. 2. Antigen retrieval:The fixation process can sometimes block the antigen sites, so antigen retrieval techniques may be used to expose them. Then it replaces on the slides.3. Antibody binding:Specific antibodies are applied to the tissue sample, and they bind to their corresponding antigens. 4. Visualization:An enzyme or fluorescent dye is used to visualize the antibody-antigen complex, making it visible under a microscope. IHC general applications: - Cancer diagnosis:IHC is widely used to differentiate between different types of cancer and to determine the most effective treatment. - Research:It helps researchers study protein expression patterns and understand disease mechanisms. - Other diagnostic applications:IHC can also be used to diagnose various other diseases and conditions by identifying specific proteins in tissues.
6
0
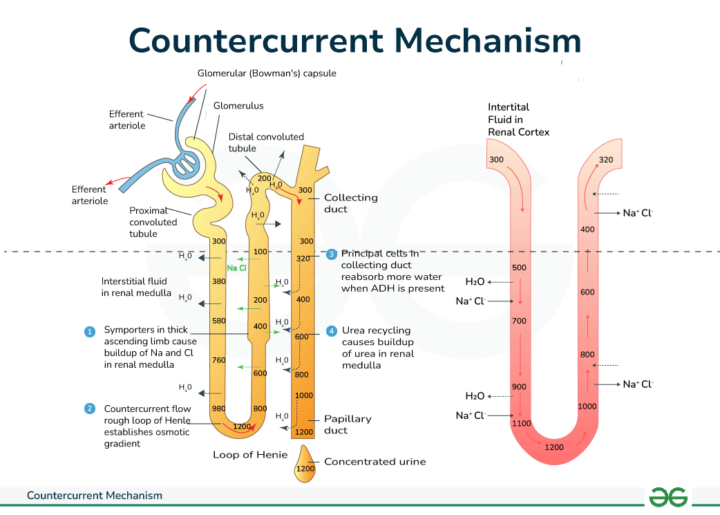
Countercurrent Multiplier Mechanism
The Loop of Henle utilizes a countercurrent multiplier mechanism to create and maintain a concentration gradient in the kidney medulla, which is essential for concentrating urine. This mechanism involves the close proximity and opposite flow of filtrate in the descending and ascending limbs of the loop of Henle, along with the vasa recta, which helps to maintain the concentration gradient. Here's a more detailed explanation: 1. Countercurrent Multiplication: - Descending Limb: The descending limb is permeable to water but relatively impermeable to salt. As the filtrate flows down this limb, water moves out into the hypertonic medullary interstitium, increasing the filtrate's concentration. - Ascending Limb: The ascending limb is impermeable to water but actively pumps out sodium and chloride ions into the medullary interstitium. This makes the filtrate more dilute and the interstitium more concentrated. - Countercurrent Flow: The opposite flow of fluid in the descending and ascending limbs (countercurrent flow) amplifies the concentration difference. The filtrate in the ascending limb is constantly pumping out salt, maintaining a high concentration in the medulla, which then draws water out of the descending limb. 2. Vasa Recta: - The vasa recta, the blood vessels surrounding the Loop of Henle, also play a role in the countercurrent system. - They have a hairpin shape, which slows down blood flow and allows for the exchange of solutes and water with the medullary interstitium. - The vasa recta help to prevent the washout of solutes from the medulla, maintaining the concentration gradient. 3. Urine Concentration: - The hypertonic medullary interstitium created by the countercurrent multiplier mechanism allows for the reabsorption of water from the collecting ducts as they pass through the medulla. - This process enables the kidneys to produce concentrated urine, conserving water for the body.
4
0
1-10 of 35
Active 2d ago
Joined Apr 16, 2025



