3d • General discussion
13. The Fallacy of Profit as the Primary Driver
When Treatment Is Shaped More by Reimbursement Than by Biology
Modern medicine operates within an economic framework that inevitably influences research priorities, therapeutic development, clinical guidelines, and patient autonomy. While financial sustainability is necessary for innovation, a growing body of evidence demonstrates that when profit becomes the primary driver, biological truth and patient-centered care can become secondary. This paper examines the structural mechanisms through which reimbursement models and commercial incentives distort research agendas, drug approval pathways, treatment guidelines, and clinical decision-making. The evidence reveals a fundamental tension: healing follows the logic of biology; commerce follows the logic of return on investment.
1. Distortion of Research Priorities
Biomedical research funding is disproportionately allocated toward patentable pharmaceutical products rather than prevention, lifestyle interventions, or non-proprietary therapies.
Industry Influence on Research Funding
Pharmaceutical companies fund approximately half of clinical trials globally (Emanuel et al., 2003; Moses et al., 2015). Industry-sponsored trials are significantly more likely to report positive outcomes compared to independently funded trials (Lundh et al., 2017, Cochrane Review). This phenomenon—publication bias and outcome reporting bias—skews the scientific literature toward commercially favorable results.
Furthermore, diseases with strong market potential (chronic conditions requiring lifelong medication) receive far greater investment than preventive strategies or curative interventions. For example, pharmaceutical development overwhelmingly prioritizes chronic management drugs over research into lifestyle-based disease reversal, despite evidence that conditions such as type 2 diabetes and cardiovascular disease are strongly modifiable through diet and behavioral interventions (Knowler et al., 2002; Ornish et al., 1998).
Economic logic favors lifelong customers. Biological logic favors restoration.
2. Distortion of Drug Approval Pathways
Surrogate Endpoints and Accelerated Approvals
Regulatory agencies such as the U.S. Food and Drug Administration increasingly rely on surrogate endpoints—biomarkers rather than clinical outcomes—for drug approvals (Downing et al., 2014). While surrogate markers can expedite approval, they do not always translate into improved survival or quality of life.
The 2021 approval of aducanumab for Alzheimer’s disease by the U.S. Food and Drug Administration was based on reduction of amyloid plaques rather than demonstrated cognitive improvement, despite significant controversy among advisory panel members (Alexander et al., 2021, JAMA). The decision raised concerns about regulatory capture and financial pressure in high-revenue therapeutic areas.
Regulatory Capture
Regulatory capture refers to a situation in which regulatory agencies become overly aligned with industry interests. Research has shown frequent financial relationships between FDA advisory committee members and pharmaceutical companies (Pham-Kanter, 2014). Additionally, the Prescription Drug User Fee Act (PDUFA) allows industry fees to fund a substantial portion of FDA drug review processes, potentially creating institutional financial dependence (Carpenter et al., 2008).
When approval timelines are financially incentivized, biology may yield to market acceleration.
3. Distortion of Treatment Guidelines
Clinical guidelines heavily influence reimbursement, insurance coverage, and physician behavior. However, conflicts of interest are common among guideline authors.
A landmark study published in BMJ found that a majority of guideline panel members had financial ties to pharmaceutical companies whose products were under consideration (Neuman et al., 2011). These financial relationships correlate with more favorable recommendations toward sponsor products.
For example:
- Expanded diagnostic criteria (e.g., lowering thresholds for hypertension or hyperlipidemia) increase the eligible treatment population.
- Widened definitions can create “pre-disease” categories that dramatically expand pharmaceutical markets (Moynihan et al., 2013).
The expansion of disease definitions does not necessarily reflect worsening biology—it may reflect expanding markets.
4. Reimbursement Structures and Procedural Bias
Healthcare systems often reimburse procedures and pharmaceuticals at significantly higher rates than lifestyle counseling, preventive education, or time-intensive relational care.
In fee-for-service systems, clinicians are incentivized toward billable interventions rather than root-cause exploration. Studies have demonstrated that primary care physicians face time constraints that limit lifestyle counseling despite strong evidence for its effectiveness (Yarnall et al., 2003).
The economic architecture subtly teaches:
- Prescribe rather than prevent.
- Intervene rather than educate.
- Manage rather than restore.
Biology favors regulation and terrain correction. Reimbursement favors intervention volume.
5. Impact on Patient Autonomy
Direct-to-consumer pharmaceutical advertising—legal only in the United States and New Zealand—shapes patient demand. The U.S. alone spends billions annually on pharmaceutical advertising (Schwartz & Woloshin, 2019). Advertising increases prescription rates regardless of clinical appropriateness.
Additionally, financial toxicity has become a recognized medical harm. High drug prices contribute to medication non-adherence, bankruptcy, and stress (Zafar et al., 2013). When patients are financially burdened by treatment, autonomy becomes constrained by economic pressure rather than guided by informed choice.
Commerce promotes demand creation. Healing requires discernment.
6. The Divergent Logics of Healing and Commerce
Biology operates according to principles of:
- Homeostasis
- Energy efficiency
- Self-repair
- System integration
- Adaptation
Commerce operates according to:
- Market expansion
- Return on investment
- Patent exclusivity
- Recurring revenue
- Competitive positioning
These logics are not inherently evil—but they are fundamentally different.
When commerce dominates, medicine can drift from supporting innate regulation toward sustaining dependency.
7. Conclusion
The evidence demonstrates that financial incentives measurably influence:
- Research agendas
- Publication patterns
- Regulatory approvals
- Clinical guidelines
- Treatment prevalence
This does not imply that all pharmaceutical innovation is corrupt or without benefit. Rather, it affirms a structural reality: economic forces shape medical practice in ways that do not always align with biological wisdom or patient-centered restoration.
Healing and commerce follow very different logics.
A biologically grounded model of medicine must evaluate interventions not only for profitability or market expansion, but for their capacity to restore regulation, reduce dependency, and strengthen the organism’s inherent design.
True medicine requires that biology—not reimbursement—remain the primary driver.
Selected References
- Alexander, G. C., et al. (2021). Revisiting FDA approval of aducanumab. JAMA.
- Carpenter, D., et al. (2008). Drug-review deadlines and safety problems. New England Journal of Medicine.
- Downing, N. S., et al. (2014). Clinical trial evidence supporting FDA approval of novel therapeutics. JAMA.
- Emanuel, E. J., et al. (2003). Financial relationships between industry and clinical investigators. NEJM.
- Knowler, W. C., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention. NEJM.
- Lundh, A., et al. (2017). Industry sponsorship and research outcome. Cochrane Database of Systematic Reviews.
- Moynihan, R., et al. (2013). Preventing overdiagnosis. BMJ.
- Moses, H., et al. (2015). The anatomy of medical research. JAMA.
- Neuman, J., et al. (2011). Financial conflicts of interest in clinical guidelines. BMJ.
- Ornish, D., et al. (1998). Intensive lifestyle changes for coronary heart disease. JAMA.
- Schwartz, L. M., & Woloshin, S. (2019). Medical marketing in the United States. JAMA.
- Yarnall, K. S., et al. (2003). Time needed to provide recommended preventive services. American Journal of Public Health.
- Zafar, S. Y., et al. (2013). Financial toxicity in cancer care. Oncology.
0
0 comments
powered by
skool.com/true-medicine-3260
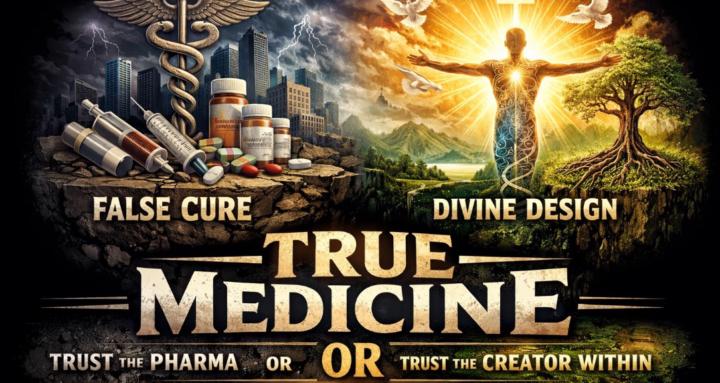
Revelation of Innate intelligence or the human body -contradicting big pharma and modern medicines hypothesis that we need their "magic" to heal.
Suggested communities
Powered by
